U.S. pregnancy-related deaths have reached alarming levels, with the nation consistently recording the highest maternal mortality rate among high-income countries. According to recent studies, a significant portion of these fatalities, over 80%, are preventable with improved prenatal and postpartum care. Despite advances in healthcare, the maternal mortality rate continues to rise, particularly between 2018 and 2022, highlighting pressing healthcare disparities across racial and geographic groups. The findings reveal an urgent need to address pregnancy complications and to reform our healthcare system to ensure equitable access to comprehensive pregnancy health services. As we examine the startling statistics surrounding mortality during and after pregnancy, the conversation shifts toward effective solutions to reduce these tragic outcomes and promote better maternal health for all.
The crisis of maternal health in the U.S. is underscored by an increasing number of pregnancy-related fatalities, often referred to as maternal mortality. This issue not only reflects the challenges of pregnancy complications but also points to a broader systemic problem within healthcare that exacerbates discrepancies in care. Furthermore, the focus on enhancing postpartum care is crucial, as many deaths can occur in the months following childbirth. Addressing healthcare disparities is paramount to improving these troubling statistics, as they disproportionately affect marginalized communities. It is vital to foster a more inclusive approach to pregnancy health, emphasizing the importance of a robust healthcare framework that supports women throughout their entire reproductive journey.
The Alarming Rise of U.S. Pregnancy-Related Deaths
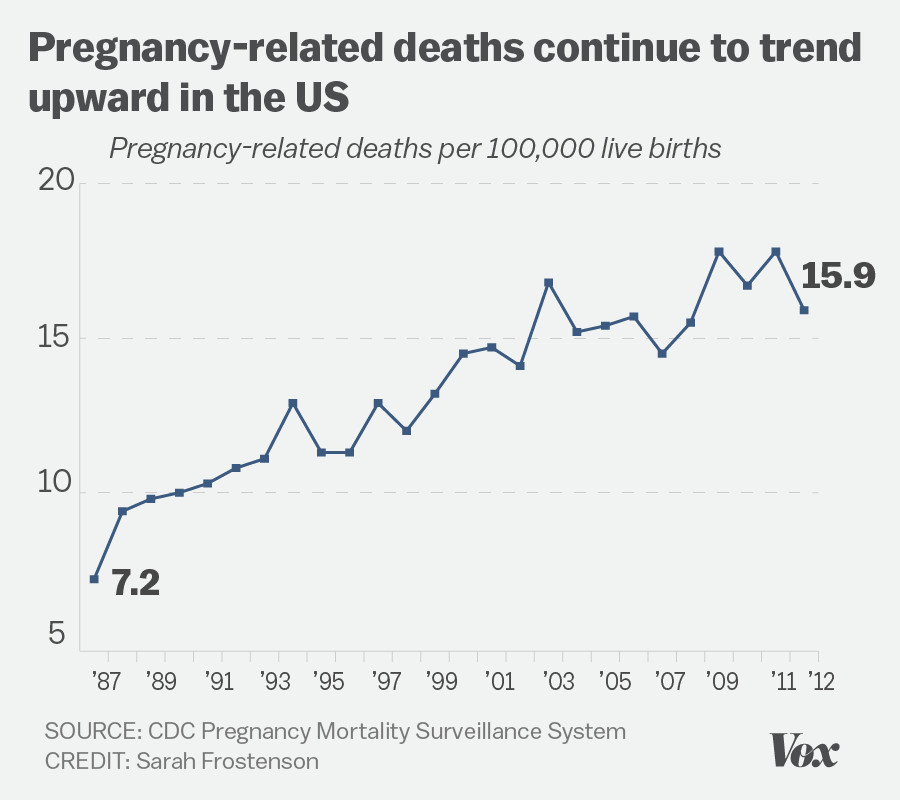
The United States has witnessed a troubling increase in pregnancy-related deaths over the past several years, asserting its position as the nation with the highest maternal mortality rate among high-income countries. Despite advancements in medical science, more than 80% of these deaths are deemed preventable. A study conducted by researchers from the National Institutes of Health highlighted significant disparities across various demographics, with alarming statistics indicating that American Indian and Alaska Native women experience mortality rates nearly four times higher than their white counterparts. This inequity underscores the urgent need for systemic changes in the healthcare infrastructure, particularly in maternal health services.
Moreover, the rise in pregnancy-related deaths is not merely a statistic; it reflects deep-rooted issues within the healthcare system. The COVID-19 pandemic was a contributing factor to this alarming trend, as seen in the spike in mortality rates in 2021. The persistence of racial and geographic disparities further exacerbates the situation. For example, while certain states report mortality rates as low as 18.5 per 100,000 live births, others witness figures soaring above 59.7. Such disparities in care access and quality indicate a pressing need for targeted policies that ensure equitable healthcare for all expecting mothers.
Critical Factors Contributing to Maternal Mortality Rates
Several factors contribute to the high maternal mortality rate in the U.S., including a fragmented healthcare system, healthcare disparities, and chronic medical conditions affecting younger populations. One prominent issue is the prevalence of chronic health conditions such as hypertension and cardiovascular disease, which have increasingly become risks during pregnancy. As more reproductive-age individuals present with chronic ailments, the risks associated with pregnancy intensify. This shift in health trends necessitates a reevaluation of how maternal care is provided, emphasizing preventive measures to address these conditions before, during, and after pregnancy.
Additionally, systemic issues such as maternity care deserts—areas lacking adequate healthcare facilities—contribute to the challenges faced by pregnant individuals. Many women encounter substantial barriers to accessing quality prenatal and postpartum care, resulting in delayed treatment for complications that could otherwise be managed effectively. Experts argue that a holistic approach to maternal health must prioritize not just pregnancy and childbirth, but also the extended postpartum period, addressing both psychological and physical health needs. This requires significant investment in healthcare infrastructure that promotes continuity of care long after childbirth.
Addressing Racial Disparities in Maternal Health
The persistence of racial disparities in maternal mortality rates is a pressing concern for public health officials. The stark contrast between mortality rates among different racial groups highlights the systemic biases ingrained within the healthcare system. Research indicates that non-Hispanic Black women and American Indian women face significantly higher risks during pregnancy compared to white women. These disparities result from a combination of factors, including social determinants of health, access to care, and discrimination within healthcare settings. Therefore, it is vital to implement strategies that directly address these inequities in order to improve maternal health outcomes across all demographics.
Recent initiatives aimed at reducing disparities have shown promise, yet substantial work remains. Policymakers and healthcare providers must collaborate to create more inclusive healthcare frameworks that focus on the unique needs of marginalized communities. By investing in culturally competent care, community-based resources, and robust support systems, the health sector can begin to rectify the historical inequities in maternal health. This approach not only improves outcomes for mothers but also sets a foundation for healthier families and communities.
Importance of Comprehensive Postpartum Care
Postpartum care is often overlooked in maternal health discussions, yet it is crucial for ensuring the long-term health of mothers. The World Health Organization recognizes maternal mortality as a significant risk occurring up to 42 days following childbirth; however, the U.S. has started to acknowledge the importance of extending this period up to one year. Late maternal deaths—deaths occurring after that six-week postpartum mark—account for nearly a third of pregnancy-related fatalities in the United States. This statistic emphasizes the necessity for continuous healthcare support and resources for women during the postpartum phase.
Healthcare providers must adopt a more comprehensive definition of postpartum care that encompasses not only physical recovery but also psychological wellbeing. Issues like postpartum depression, anxiety, and other chronic conditions can significantly affect a new mother’s ability to care for herself and her child. Increased awareness and proactive measures in postpartum support can help mitigate these risks, ultimately leading to better health outcomes. By treating postpartum care as an integral part of maternal health, we can create a system that supports mothers holistically.
The Role of Public Health Infrastructure in Maternal Health
Investing in public health infrastructure is critical to combatting the rise in pregnancy-related deaths in the United States. The ongoing COVID-19 pandemic has illustrated the fragility of health systems, highlighting gaps in care that have serious implications for maternal health. A robust public health infrastructure would provide the necessary framework to support and improve health outcomes for pregnant individuals. This includes tracking maternal deaths effectively, identifying trends, and implementing targeted interventions across states to reduce mortality rates.
Moreover, there is a pressing need for federal and state-level investments designed to enhance the quality of care available to mothers before, during, and after pregnancy. With the alarming trend of rising mortality rates, it’s imperative to prioritize maternal health as a fundamental component of public health policy. This necessitates concerted efforts toward training healthcare professionals, increasing funding for maternal health initiatives, and developing community-based programs that support expecting mothers, particularly in underserved populations.
Investing in Quality Care to Reduce Maternal Mortality
To effectively combat the rising maternal mortality rates, a multifaceted approach focusing on quality care is essential. This encompasses not just improved prenatal care but also extends into the postpartum phase, emphasizing the continuity of care for mothers. Research has demonstrated that early intervention and sophisticated care pathways during pregnancy can significantly reduce adverse outcomes. By fostering equity in healthcare access and outcomes between different racial and socioeconomic groups, the U.S. can align itself closer with its high-income peers who maintain lower maternal mortality rates.
Innovative solutions and partnerships within the healthcare sector can help bridge existing gaps in maternity care. For instance, integrating telehealth services allows for greater accessibility, particularly in remote areas where healthcare facilities are scarce. By harnessing technology and ensuring comprehensive care—addressing both physical and mental health needs—healthcare providers can improve pregnancy health outcomes. This systemic change must be coupled with advocacy for policies that support families, including maternity leave and parental support initiatives, to ensure a healthier future for mothers and their children.
The Impact of Chronic Conditions on Maternal Mortality
Chronic conditions such as hypertension and cardiovascular disease have emerged as significant contributors to maternal mortality in the United States. As the prevalence of these conditions rises among younger populations, understanding their impact on pregnancy becomes increasingly crucial. Hypertension, in particular, has transitioned from a less prominent concern to one of the leading causes of pregnancy-related deaths. Education and prevention strategies targeting these chronic diseases must be incorporated into prenatal care protocols to address these risks effectively.
Furthermore, health care systems must adapt their approaches to focus on the underlying factors that lead to the exacerbation of chronic conditions during pregnancy. This includes routine screening for cardiovascular health early in pregnancy and ensuring women at risk receive the necessary interventions. Public health campaigns aimed at raising awareness about the risks associated with these conditions during pregnancy can empower women to seek early and consistent healthcare—ultimately leading to better maternal health outcomes.
Leveraging Data to Improve Maternal Health Outcomes
Data collection and analysis play a pivotal role in addressing maternal mortality issues in the United States. For decades, a lack of consistent tracking of pregnancy-related deaths hindered the ability to formulate effective public health strategies. The implementation of a national system for tracking these deaths, initiated in 2018, marks a significant step towards understanding the scope of maternal mortality. Continuous data analysis will enable health officials to identify patterns and disparities, informing targeted interventions that can effectively reduce the mortality rate.
Moreover, leveraging data to identify at-risk populations can enhance the tailoring of maternal health programs. By understanding the unique socioeconomic, racial, and geographic factors that contribute to mortality, policymakers can implement strategies that prioritize the most vulnerable groups, ensuring resources are allocated where they are most needed. As the nation grapples with rising mortality rates, the use of data-driven approaches will be essential in guiding effective public health responses and promoting healthy pregnancies.
Collaboration for Better Maternal Health Policies
Collaboration among various stakeholders is vital to formulating effective maternal health policies that can lead to substantial improvements in outcomes. This includes not only healthcare providers but also community organizations, policymakers, and advocates fighting for maternal health improvements. By engaging multifaceted partnerships, we can create comprehensive campaigns focusing on the prevention of maternal mortality and the promotion of equitable health care. Joining forces allows for pooling of resources, expertise, and knowledge aimed at fostering systemic changes in maternal health.
Additionally, enhancing awareness of maternal health disparities and advocating for policy changes are crucial. Policymakers can play a transformative role by prioritizing maternal health funding, developing initiatives to reduce healthcare inequities, and addressing social determinants that affect access to care. By creating environments that support families and ensure proper postpartum care, we can make strides toward significantly reducing the maternal mortality rate in the U.S. It is through unified efforts that we can hope to see a decline in pregnancy-related deaths and a healthier future for mothers and children alike.
Frequently Asked Questions
What factors contribute to the high U.S. pregnancy-related deaths compared to other high-income countries?
The high U.S. pregnancy-related deaths are attributed to a fragmented healthcare system, inequitable policies, and a lack of access to necessary prenatal and postpartum care. Additionally, systemic biases in treatment across different racial and ethnic groups further exacerbate the maternal mortality rate.
What is the maternal mortality rate in the U.S. and how has it changed recently?
The current maternal mortality rate in the U.S. has increased from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. This rise reflects worsening health outcomes not only during pregnancy but also in the postpartum period, highlighting the need for improved pregnancy health systems.
How do healthcare disparities affect pregnancy complications in the U.S.?
Healthcare disparities significantly impact pregnancy complications by limiting access to quality care for marginalized groups. For instance, American Indian and Alaska Native women experience nearly four times the pregnancy-related death rate of white women, underscoring the urgent need for equitable healthcare solutions.
What role does postpartum care play in addressing pregnancy-related deaths?
Postpartum care is crucial because many pregnancy-related deaths occur post-delivery, often between 42 days and one year after birth. Improving care continuity beyond the initial postpartum phase can significantly reduce late maternal deaths and enhance overall maternal health.
How can the rise in maternal mortality rates among younger women be explained?
The increase in maternal mortality rates among younger women is linked to a rise in chronic medical conditions, like hypertension, that were traditionally more common in older populations. Effective management and awareness of these health issues during pregnancy are essential to prevent resulting complications.
What are the leading causes of pregnancy-related deaths in the U.S.?
Cardiovascular disease is the leading cause, accounting for over 20% of pregnancy-related deaths, especially due to conditions like hypertension and pre-eclampsia. This shift from hemorrhage to cardiovascular issues highlights a critical area for improvement in maternal healthcare.
What steps can be taken to reduce pregnancy-related deaths in the U.S.?
To reduce pregnancy-related deaths, there’s a need for improved public health infrastructure, increased investment in prenatal and postpartum care, and policy changes that address the disparities across different states. Effective data collection and health policy advocacy are also necessary for long-term improvements.
How do pregnancy-related death rates vary among different racial and ethnic groups?
Pregnancy-related death rates show significant racial disparities, with American Indian and Alaska Native women facing the highest mortality rates. Such disparities highlight the importance of targeted interventions that address the unique challenges different communities face in accessing maternal healthcare.
Why is it essential to include late maternal deaths in discussions about pregnancy-related mortality?
Including late maternal deaths, which occur between 42 days to a year postpartum, is essential to understand the full impact of pregnancy health. Recognizing this time frame promotes continuous care and highlights the need for a more holistic approach to postpartum recovery.
What systemic changes are needed to improve maternal health outcomes in the U.S.?
Systemic changes include enhancing the quality of maternal health care, increasing investment in research and public health initiatives, and addressing healthcare disparities to ensure equitable access to all women. A focus on innovative solutions and community engagement is vital for long-term health improvements.
| Key Points | Details |
|---|---|
| Overall U.S. Pregnancy-Related Deaths | Over 80% of pregnancy-related deaths in the U.S. are preventable. |
| Current Maternal Mortality Rate | As of 2022, the rate stands at 32.6 deaths per 100,000 live births, an increase from 25.3 in 2018. |
| Disparities by Demographics | American Indian and Alaska Native women experience the highest rates at 106.3 deaths per 100,000 live births. |
| Influence of COVID-19 | The sharpest increase in mortality occurred in 2021 likely due to the onset of the COVID-19 pandemic. |
| Leading Cause of Death | Cardiovascular disease is now the leading cause of pregnancy-related deaths, accounting for over 20%. |
| Importance of Postpartum Care | Late maternal deaths, which occur after 42 days postpartum, accounted for nearly a third of deaths. |
| Need for Policy Changes | Investment in public health infrastructure and policies addressing state-level disparities are crucial. |
Summary
U.S. pregnancy-related deaths have become an urgent public health issue, showing a troubling increase over recent years. Despite advancements in medical care, the U.S. continues to lead high-income countries in maternal mortality, with significant disparities across demographics. Immediate reforms in healthcare approaches, particularly in prenatal and postpartum care, are necessary to combat these rising rates. Addressing chronic health issues, ensuring access to quality maternal care, and implementing effective policies can turn the tide on this alarming trend.