In the pursuit of innovative Alzheimer’s disease treatment, TIM-3 therapy for Alzheimer’s stands out as a promising strategy that may revolutionize care for those afflicted by this devastating condition. Recent studies suggest that targeting the TIM-3 molecule can enhance brain immune responses, leading to significant memory improvement in mice. This innovative approach hinges on the critical role of immune system checkpoint molecules, which, when modified, enable microglia to better clear harmful plaques from the brain. By reprogramming these vital cells, researchers are paving the way to potentially halt or even reverse the cognitive decline characteristic of Alzheimer’s disease. As exploration of TIM-3 continues, the promise of improving life quality for Alzheimer’s patients grows stronger.
The fight against cognitive decline in Alzheimer’s begins to take a fresh direction with the use of TIM-3 therapy, a groundbreaking approach that targets pivotal molecular pathways. This strategy taps into the brain’s own defense mechanisms by focusing on immune cells, particularly microglia, which are crucial for clearing toxic plaques that accumulate with age. By understanding how checkpoint molecules regulate immune activity in the brain, scientists are developing methods to enhance memory and cognitive function, as seen in experimental models. As researchers examine ways to leverage human-specific TIM-3 antibodies, the vision of a treatment that addresses the underlying immunological aspects of Alzheimer’s becomes increasingly tangible. This revolutionary approach may redefine the landscape of Alzheimer’s disease intervention.
Introduction to TIM-3 in Alzheimer’s Disease Therapy
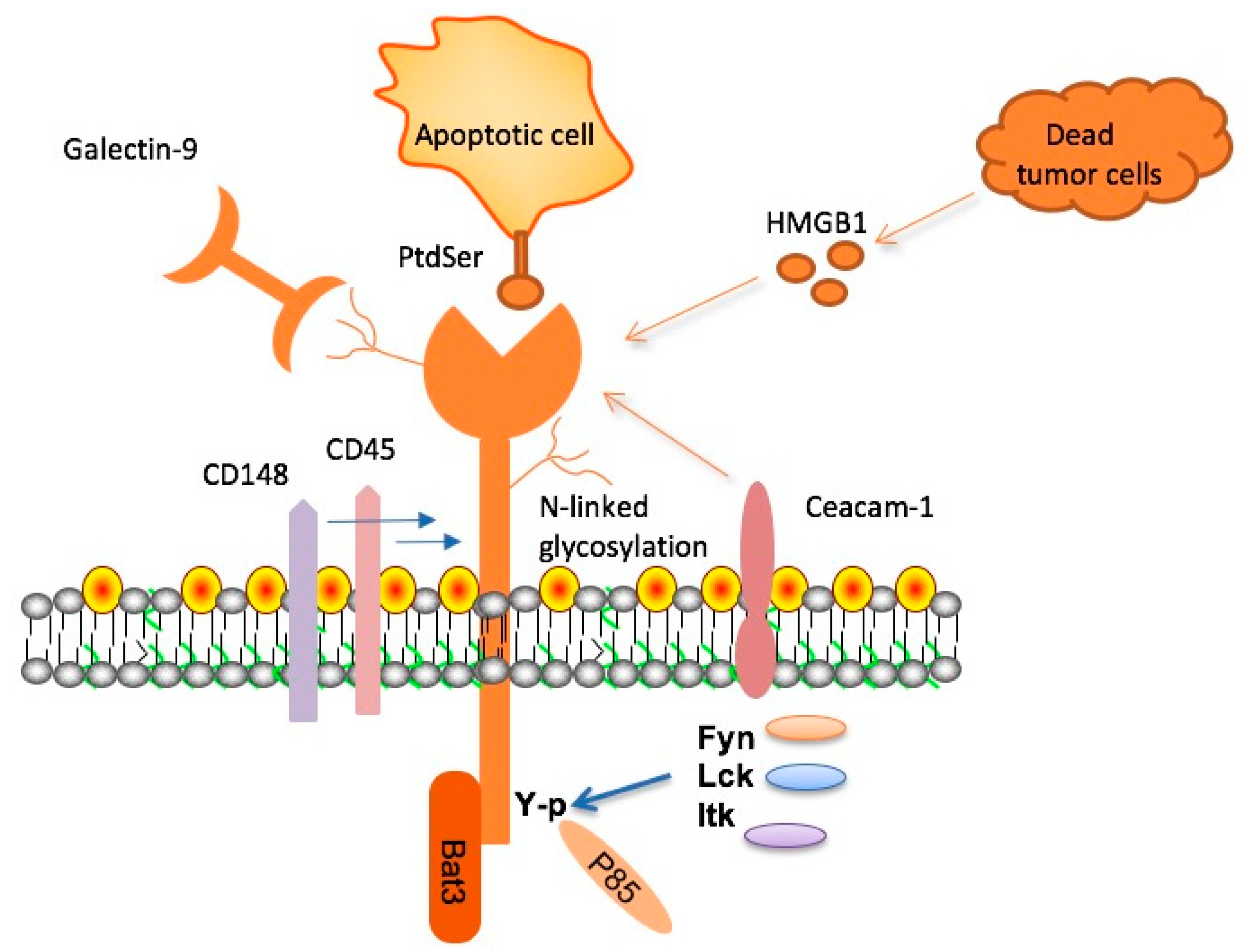
Recent studies have shown a promising connection between TIM-3 therapy and potential treatments for Alzheimer’s disease. TIM-3 is an immunological checkpoint molecule traditionally associated with tumors. By inhibiting TIM-3, researchers have discovered that microglia, the brain’s resident immune cells, can become more active in clearing amyloid plaques associated with Alzheimer’s. This breakthrough may open new avenues for tackling Alzheimer’s disease treatment, which has been a daunting challenge in the medical field.
Alzheimer’s disease, largely characterized by the buildup of amyloid-beta plaques in the brain, affects millions worldwide. As we delve into innovative therapies, TIM-3 presents a dual function: it acts as a regulator of immune responses while simultaneously being a barrier to effective plaque clearance. Researchers are now focusing on harnessing TIM-3 modulation to unleash microglial activity, potentially leading to enhanced cognitive functions and improved memory in patients.
Understanding the Role of Microglia in Alzheimer’s
Microglia serve as critical players in the brain’s immune defense system. They continually monitor the brain environment for pathogens, damaged cells, and plaques. In Alzheimer’s disease, however, these microglia become less effective due to elevated expression of checkpoint molecules such as TIM-3, which inhibits their function. The relationship between microglia and TIM-3 in the context of Alzheimer’s is significant as it suggests that by reducing TIM-3 expression, we may enhance microglial function and improve plaque clearance.
The dysfunction of microglia contributes significantly to the progression of Alzheimer’s disease, as their ability to phagocytize amyloid plaques diminishes. This failure is in part due to the immunosuppressive environment fostered by TIM-3. By focusing on therapies that can modulate the activity of microglia through TIM-3 inhibition, researchers aim to restore this crucial immune response. Improved understanding of microglial dynamics might lead to innovative Alzheimer’s disease treatments that actively target underlying neuroinflammation and enhance cognitive wellbeing.
Checkpoint Molecules: Therapeutic Potential in Alzheimer’s
Checkpoint molecules, such as TIM-3, play a fundamental role in maintaining immune balance. While they are essential for preventing tissue damage from overactive immune responses, their upregulation can impede necessary immune functions in neurological disorders like Alzheimer’s. Targeting checkpoint molecules presents a unique therapeutic angle; therapies that inhibit TIM-3 function could potentially unleash microglial activity to combat plaque accumulation, paving the way for memory improvement in affected individuals.
Recent developments have shown that restoring the functionality of immune cells through TIM-3 inhibition may create a robust strategy for tackling neurodegeneration in Alzheimer’s. By allowing microglia to effectively engage with amyloid plaques, these therapies may not only decrease plaque volume but also improve synaptic health. Exploring the therapeutic impact of checkpoint molecule interference in Alzheimer’s could redefine the course of current treatments and bring forth a wave of new approaches.
The Path to Enhancing Memory Through TIM-3 Therapy
One of the goals of TIM-3 therapies is to enhance memory by improving cognitive functions in affected individuals. Preclinical tests in mouse models have shown that deleting the TIM-3 gene allows for more robust microglial activity, resulting in reduced plaque load and improvement in memory-related tasks. This memory restoration effect highlights the potential for TIM-3 therapy to not only halt disease progression but also ameliorate existing cognitive deficits.
Improvements in cognitive behavior observed in laboratory mice suggest that TIM-3 therapy could trigger significant advancements in Alzheimer’s disease treatment. As researchers work towards translating these findings into human applications, there is optimism that therapies targeting TIM-3 may restore some degree of memory function in Alzheimer’s patients, offering hope amidst a landscape where previous treatments have largely underperformed.
Future Directions for Alzheimer’s Research
The future of Alzheimer’s research is promising, particularly with regards to TIM-3 therapies. Ongoing studies involve investigating the possibility of using anti-TIM-3 antibodies to stop plaque development in models that mirror human Alzheimer’s disease. Insights gained from these studies could lead to breakthroughs in how we understand and treat this complex neurodegenerative disorder, potentially making significant strides towards enhancing patient care.
With the introduction of genetic modifications that allow for studying human-like TIM-3 activity in mouse models, the implications for future therapeutics are vast. If successful, these therapies could lay the groundwork for innovative interventions that effectively tackle Alzheimer’s disease through immune modulation. The potential to repurpose existing cancer therapies targeting TIM-3 for Alzheimer’s opens new doors that may redefine therapeutic strategies in the battle against Alzheimer’s.
Challenges and Considerations in TIM-3 Therapy
While the prospects for TIM-3 therapy in Alzheimer’s disease are promising, there are inherent challenges in developing successful strategies. The delicate balance of immune modulation must be carefully managed to avoid unintended consequences, such as excessive inflammation or autoimmunity. Tailoring TIM-3 inhibition specifically for neurodegenerative pathways will require intensive research to ensure efficacy and safety.
Furthermore, translating findings from animal models to human treatment poses its own set of hurdles. Variability in patient response based on genetic backgrounds, comorbid conditions, and previous treatments might influence how well TIM-3 therapy works in practice. Addressing these challenges is crucial to maximizing the therapeutic potential of TIM-3 and realizing a future where Alzheimer’s disease can be more effectively managed.
Exploring Alternative Treatments along with TIM-3 Therapy
As researchers explore TIM-3 therapy, it’s essential to consider integrating it with other Alzheimer’s disease treatments. While TIM-3 focuses on microglial activation, combinatorial therapies with anti-amyloid agents could provide a holistic approach to tackle plaque accumulation and neuroinflammation concurrently. This multi-faceted strategy may lead to more profound cognitive improvements by addressing multiple pathways involved in Alzheimer’s disease.
Integrating various treatment modalities alongside TIM-3 therapy could produce synergistic effects. For instance, alongside immunotherapy, lifestyle modifications, nutritional support, and cognitive training may enhance patient outcomes. The future of Alzheimer’s care will likely encompass comprehensive treatment plans that leverage innovations in immunology, neurobiology, and personalized medicine to create individualized strategies for managing Alzheimer’s.
Implications of TIM-3 on Future Alzheimer’s Disease Studies
The discussions surrounding TIM-3 therapy have broad implications beyond its immediate effects on Alzheimer’s disease. The insights gained from studying this checkpoint molecule may expand our understanding of immune responses in the brain and influence approaches to treating other neurological disorders. As research progresses, TIM-3 could emerge as a key player in the neural immune interface, with ramifications that extend into various fields of medicine.
Engaging with the complexities of TIM-3 and its role offers vital lessons for future Alzheimer’s research, emphasizing the need for innovative thinking in drug development. As we learn more about how TIM-3 influences microglial activity, we may uncover new biomarkers for disease progression, leading to early diagnosis and intervention strategies that target underlying pathology more effectively.
Conclusion: The Future of Alzheimer’s Treatment is Within Reach
The exploration of TIM-3 therapy for Alzheimer’s disease signifies a pivotal moment in the pursuit of effective treatments. With the potential to modify immune responses in the brain, TIM-3 could create new paradigms in how we approach Alzheimer’s disease treatment. As the research community continues to unravel the complexities behind TIM-3 and its impact, there’s hope that a functional therapy will emerge that improves the quality of life for countless individuals suffering from Alzheimer’s.
In summary, the intersection of immunology and neurology through TIM-3 therapy sheds light on the many avenues still to be explored in Alzheimer’s disease research. As we advance in our scientific understanding and therapeutic strategies, the foundation laid today could lead to groundbreaking treatments that enhance not only cognitive health but also the overall well-being of those affected by Alzheimer’s.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease?
TIM-3 therapy for Alzheimer’s disease involves targeting the TIM-3 checkpoint molecule, which inhibits microglia from clearing amyloid plaques in the brain. By blocking TIM-3, studies have shown that microglia can resume their role in attacking these plaques, potentially restoring memory function and slowing the progression of Alzheimer’s.
How does TIM-3 affect the immune system in Alzheimer’s treatment?
In Alzheimer’s treatment, TIM-3 acts as an inhibitory checkpoint molecule that prevents microglia from attacking amyloid plaques in the brain. By inhibiting TIM-3, researchers aim to enhance the immune response of microglia, allowing them to clear plaques associated with Alzheimer’s disease more effectively, which may lead to improved cognitive function.
Can TIM-3 therapy improve memory in Alzheimer’s patients?
Yes, TIM-3 therapy shows promise in improving memory by enhancing the ability of microglia to clear amyloid plaques from the brain. Studies have demonstrated that deleting TIM-3 expression in mouse models led to significant improvements in cognitive function, suggesting a potential pathway for memory improvement in Alzheimer’s patients through similar therapies.
What role do checkpoint molecules like TIM-3 play in Alzheimer’s disease?
Checkpoint molecules like TIM-3 are crucial in regulating immune responses. In the context of Alzheimer’s disease, TIM-3 prevents microglia from clearing harmful amyloid plaques, contributing to the progression of the disease. Targeting TIM-3 may reverse this inhibition, restoring microglial function and facilitating the clearing of plaques.
What are microglia and their significance in TIM-3 therapy for Alzheimer’s?
Microglia are the brain’s immune cells, responsible for maintaining homeostasis and clearing waste products like amyloid plaques. In TIM-3 therapy for Alzheimer’s, these cells are critical because inhibiting TIM-3 can release them from their restrained state, enabling them to attack and clear accumulated plaques that impair cognitive function.
What is the potential impact of TIM-3 therapy on Alzheimer’s disease treatment?
The potential impact of TIM-3 therapy on Alzheimer’s disease treatment is significant, as it could offer a novel approach to enhance the immune response against plaque accumulation. This strategy may lead to breakthroughs in cognitive improvement, especially after challenges faced in previous Alzheimer’s drug trials, offering hope for better therapeutic outcomes.
How does TIM-3 relate to late-onset Alzheimer’s disease?
TIM-3 has been linked to late-onset Alzheimer’s disease as a genetic risk factor. Studies have shown that variants of the TIM-3 gene (HAVCR2) are more prevalent in individuals with late-onset Alzheimer’s, indicating that targeting TIM-3 may be a promising avenue for treatment in this most common form of the disease.
What are the next steps for TIM-3 therapy in humans?
The next steps for TIM-3 therapy in humans involve testing human anti-TIM-3 antibodies in mouse models of Alzheimer’s disease. Researchers aim to evaluate their efficacy in halting plaque development, paving the way for clinical trials and potential therapeutic applications for Alzheimer’s patients.
| Key Point | Details |
|---|---|
| Research Background | A new study suggests TIM-3, an immune checkpoint molecule, may aid in treating Alzheimer’s disease by enhancing microglial function. |
| Role of TIM-3 | TIM-3 is linked to late-onset Alzheimer’s and inhibits microglia from clearing amyloid plaques. |
| Microglia Function | Microglia are brain immune cells that help prune unused synapses and clear plaques, but TIM-3 inhibits this function with age. |
| Experimental Findings | In TIM-3 deficient mice, there was improved plaque clearance and cognitive restoration, as measured by maze navigation. |
| Therapeutic Approach | Potential treatments may involve anti-TIM-3 antibodies to enhance microglial activity in humans. |
| Future Research | Ongoing studies aim to assess the effectiveness of human anti-TIM-3 gene therapy in Alzheimer’s mouse models. |
Summary
TIM-3 therapy for Alzheimer’s is emerging as a promising treatment strategy aimed at enhancing cognitive function by modulating brain immune responses. This innovative approach leverages insights from cancer treatment, focusing on the TIM-3 molecule’s role in regulating microglial cells, which are crucial for clearing amyloid plaques. Early studies indicate that inhibiting TIM-3 may restore the ability of microglia to combat plaque buildup, thereby improving cognitive performance in affected individuals. As research progresses, TIM-3 therapy could pave the way for novel interventions in the fight against Alzheimer’s disease.